Best Practices for Therapy Notes Documentation
Documenting Gray Areas: Risk Assessment for “Medium Risk” Clients
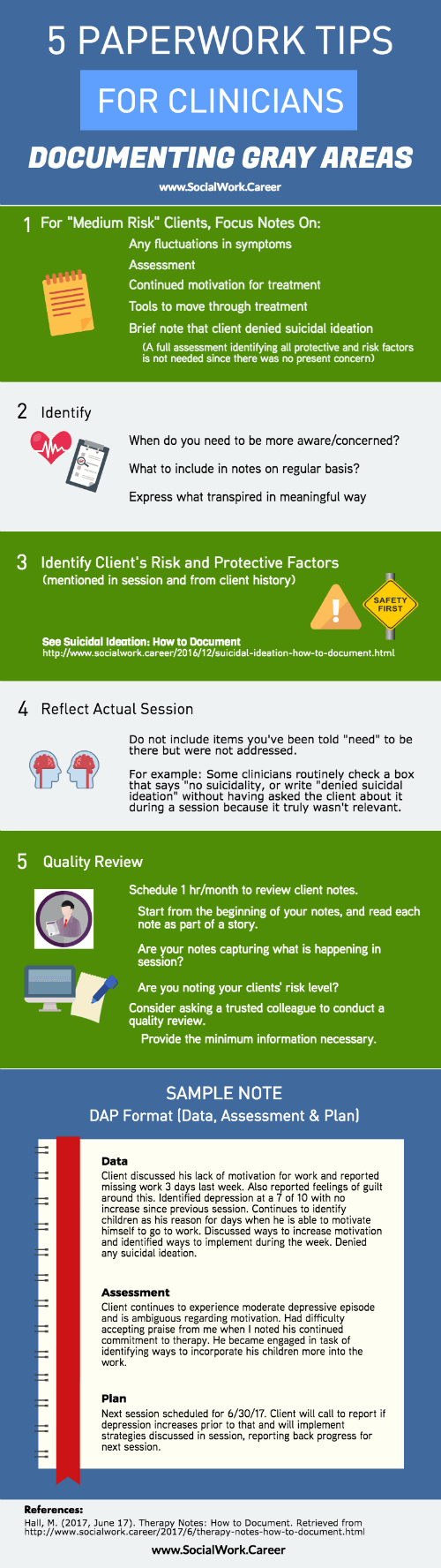
Therapy notes documentation can be challenging when clients fall into gray areas, not quite high-risk but requiring more attention than low-risk cases. These “medium risk” situations include clients with ongoing depression, self-harm behaviors, impulsivity, and substance use. This guide provides five expert tips for documenting these cases effectively without overwhelming yourself with paperwork.
All counselors understand that high risk situations, such as a client reporting suicidal thoughts, require significant and timely therapy notes documentation. However, what about the gray areas we encounter on a daily basis? The situations that linger and don’t quite meet the “high risk” threshold?
That’s exactly what we’ll be discussing in this post – what to write for your “medium risk” clients who don’t keep you up at night worrying about their outcome, but also don’t leave you worry-free each week.
Now, I want to start by saying that I do NOT take the approach of wanting to scare everyone into writing excessive amounts of therapy notes, as you may have heard when attending workshops run by lawyers or malpractice insurance organizations. Many clinicians are used to an all-or-nothing approach where they either write very little or feel as though they need a transcript of what happened in the session.
The key is identifying when you need to be more aware, what to include in your notes on a regular basis, and how to make your notes express what transpired in a meaningful way.
It’s also important to have an approach that allows you to write in the long-term. While crisis sessions tend to be a significant event that then winds down over time, medium risk situations can last for quite a while. That’s why having a realistic approach that covers all your legal and ethical bases, while also allowing you to get your therapy notes done in a reasonable timeframe is important.
Defining Medium Risk
Many clinicians struggle with therapy notes documentation for medium risk clients.
First, let’s define what we mean by “medium risk” situations. These tend to be ongoing needs that require some assessment but in which the outcome is not likely to be severe enough to require a report or hospitalization.
Some examples of medium risk presentations include:
- Self-harm behaviors not identified as related to suicidal ideation
- Moderate and severe depression
- Impulsivity and adrenaline-seeking behaviors
- Substance use
Therapy Notes Documentation: 5 Tips for Clinicians
Identify What is Relevant
As discussed in Suicidal Ideation: How to Document on assessing suicide risk, you’ll want to make sure you include in your therapy notes details along the way that shows an ongoing assessment of risk factors, protective factors and safety planning. However, since these situations tend to be more chronic than acute, it may be fine to reference previously obtained information or situations, rather than constantly writing everything out in each note.
For example, if you’re working with a client who is expressing moderate depression, you’ll want to continue assessing their symptoms to ensure you’re aware of any increase. However, if they’ve never expressed suicidality, you may not need to do a risk assessment every session.
Please note that I do recommend you ask every client about any history of or current thoughts related to suicidality when you begin treatment, particularly if the client presents with depressed mood. Based on that information you gather, you will then determine how to best proceed.
If you do feel it is necessary to include information about denial of suicidal ideation in each note for a period of time, it can simply be a brief note rather than a full account of the risk assessment. Of course, these are circumstances in which you want to use your clinical judgment, but I advise against treating each client exactly the same.
Document what is relevant for each client and if suicidal ideation has never been an issue, there is no reason to write about it in every client note. In fact, I would not write about it unless you actually asked or assessed the client. Many clinicians will routinely check a box that says “No suicidality” or will write “Denied suicidal ideation” without even asking the client about it during that session… because it truly wasn’t relevant.
One scenario may be a client who is seeing you for stress related to work, has never expressed any suicidal ideation (and denied it during your first sessions), is making vast improvements and is now only seeing you twice per month. This client does not need a regular note about this because she is low risk and most clinicians are not actually discussing the topic of suicidal ideation with her each session.
Basic rule: keep your notes to what you actually do in session! Don’t include random things others may have told you “need” to be there but don’t actually relate to what you’ve done.
Review a Real Note
That probably sounds too simple, but let’s explore further for our medium risk clients. So, what would therapy notes documentation for a medium risk client actually look like? Let’s look at an example.
Below is an example using the DAP (Data, Assessment, Plan) template for writing therapy notes. This note is for an imaginary client who is a 36 year old male that reports being depressed “for most of my adult life” at intake and currently has no motivation to work:
Data: Client discussed his lack of motivation for work and reported missing work 3 days last week. Also reported feelings of guilt around this. Identified depression at a 7 of 10 with no increase since previous session. Continues to identify children as his reason for days when he is able to motivate himself to go to work. Discussed ways to increase motivation and identified ways to implement during the week. Denied any suicidal ideation.
Assessment: Client continues to experience moderate depressive episode and is ambiguous regarding motivation. Had difficulty accepting praise from me when I noted his continued commitment to therapy. He became engaged in task of identifying ways to incorporate his children more into the work.
Plan: Next session scheduled for 6/30/17. Client will call to report if depression increases prior to that and will implement strategies discussed in session, reporting back progress for next session.
This therapy note focuses on any fluctuations in symptoms, an assessment of the present condition, continued motivation for treatment and identifying tools to move through treatment. The focus is on his actual treatment and the presentation related to that.
The note mentions that the client denied suicidal ideation, since his depression is continuing to be monitored. However, a full assessment identifying all protective and risk factors is not needed since there was no present concern.
One Quick Tip
Lastly, these scenarios speak to two crucial things that are important but often overlooked in private practice settings- having other clinicians review your therapy notes documentation and reviewing your own notes regularly.
I always recommend that clinicians schedule just one hour per month (or even every other month) to review client notes. That means sitting down with the file or at your computer, starting with the beginning, and reading each note as a story.
Ask yourself if your therapy notes documentation seem to capture what you feel is happening in session. This is also a great opportunity to realize when you may be missing something important, or to identify trends that may not be so apparent when you’re in the day to day work.
You’ll also quickly be able to recognize if you are documenting the risk level for your clients. And if it is hard to tell? That’s when you ask a trusted colleague to do a review for you. Note that quality reviews are covered under HIPAA, meaning that it is acceptable to allow a colleague to do so. However, you’ll want to make sure you are only providing the minimum necessary (if you can hide names and other info, that’s ideal) and that you are working with a colleague you know and trust.
Ask them to explain the case to you after reading through it and whether or not they have questions. This will help you see any blind spots you have and if what is happening in the room is making it to paper.
This approach to therapy notes documentation saves time while maintaining quality. Using the strategies above should help you to actually save time on documentation in the long run, while still making it a meaningful part of the treatment that fulfills your ethical obligations.
Like this post? Please share it!
About the Author: Maelisa Hall, Psy.D. specializes in teaching therapists how to connect with their paperwork so it’s more simple and more meaningful. The result? Rock solid documentation every therapist can be proud of! Check out her free online Private Practice Paperwork Crash Course, and get tips on improving your documentation today.
Frequently Asked Questions
What are medium risk clients in therapy?
Medium risk clients present ongoing concerns that require assessment but typically don’t need immediate crisis intervention. Examples include clients with moderate to severe depression, self-harm behaviors not related to suicidal ideation, impulsivity, adrenaline-seeking behaviors, and substance use. These situations are chronic rather than acute, lasting weeks or months rather than days.
Do I need to document suicidal ideation in every therapy note?
No. Only document what you actually assess during the session. If a client has never expressed suicidal ideation and is low-risk (such as someone seeing you for work stress), there’s no need to routinely note “denied suicidal ideation” unless you specifically asked about it. Document what’s clinically relevant for each individual client rather than using a one-size-fits-all approach.
What is the DAP format for therapy notes?
DAP stands for Data, Assessment, and Plan. Data includes what the client reported and observed behaviors. Assessment covers your clinical impressions and the client’s current condition. Plan outlines next steps, including scheduled appointments and agreed-upon strategies. This format provides a clear, organized structure for documenting therapy sessions.
How often should I review my therapy notes?
Review your client notes for one hour every month or every other month. Read through each note from beginning to end as a story. This helps you identify trends, ensure you’re capturing what happens in sessions, recognize missing information, and assess whether you’re documenting risk appropriately. Consider having a trusted colleague review your notes periodically for additional perspective.
What should I include in notes for clients with depression?
For clients with moderate or severe depression, document fluctuations in symptoms, current depression levels (rating scales can be helpful), protective factors like motivation to attend sessions or reasons for living, ongoing assessment of any changes in risk, treatment engagement, and progress toward goals. You don’t need to conduct a full suicide risk assessment every session unless clinical judgment indicates it’s necessary.
How do I document self-harm that’s not suicidal?
Document self-harm behaviors by noting the behavior itself, the client’s stated intent or function of the behavior, frequency and recent changes, coping strategies discussed, and safety planning. Clearly differentiate between self-harm as a coping mechanism versus self-harm related to suicidal ideation. Focus on monitoring patterns and working collaboratively with the client on alternative coping skills.
What are common therapy notes documentation mistakes therapists make?
Common mistakes include documenting items not actually discussed in session, using identical templates for every client regardless of relevance, writing excessively detailed transcripts instead of focused clinical notes, failing to document medium risk situations adequately, and not reviewing notes regularly to ensure they tell a coherent story. Focus on documenting what you actually do in session and what’s clinically relevant.
Can colleagues review my therapy notes under HIPAA?
Yes. Quality reviews are covered under HIPAA as part of treatment, payment, and healthcare operations. When having a colleague review your notes, provide only the minimum necessary information—hide names and identifying details when possible. Work only with colleagues you know and trust. This peer review process helps identify blind spots and ensures your documentation accurately reflects what happens in sessions.
How detailed should therapy notes be?
Therapy notes should be detailed enough to document clinical decision-making, risk assessment, and treatment progress, but not so detailed that they become unsustainable. Avoid extremes—neither minimal notes that lack substance nor transcripts of sessions. Focus on capturing what’s clinically meaningful: changes in symptoms, risk factors, protective factors, interventions used, and the client’s response to treatment.
What is the best way to save time on therapy notes documentation?
Save time by documenting only what’s relevant to each client, using structured formats like DAP that guide your writing, avoiding unnecessary repetition across notes for chronic situations, focusing on changes rather than restating the same information each session, and creating a sustainable routine that allows you to maintain quality long-term. Efficient documentation comes from knowing what matters, not from writing less.
Last updated: January 4, 2026
Looking for more articles on suicide risk assessment or HIPAA compliance? Explore these related posts.

Hi Maelisa,
My supervisor who has a BSW told me I can’t use “appeared” when describing client affect or how the client presented…What’s your opinion on that? I was taught in grad school that word was fine.
Thanks,
Dora
Hi Dora,
Great question! I think there will always be differences in opinion about a lot of these specific things. I don’t have a strong feeling about that word one way or the other, actually. However, I think noting that a client “presented as…” is usually a good way to remain objective. Regardless of the term you use, the important part is actually describing the behavior or quote or whatever it was that makes you think the client is one way or the other.
Hope that helps!
-Maelisa
Thanks, Maelisa Hall takes the ordinary documentation blahs and turns them into a meaningful thread of exploring the client with more clarity.
I learned things I will implement immediately.
Thanks so much for sharing, Sandy!
I totally agree – Maelisa has a wonderful skill and knack at everything therapy note related! I’ll make sure to share with her your kind comment 🙂
Thanks, Sandy! It seems so easy to do these things with clients and yet difficult to implement with documentation. I’m glad to offer a few ways to make things easier AND more meaningful 🙂