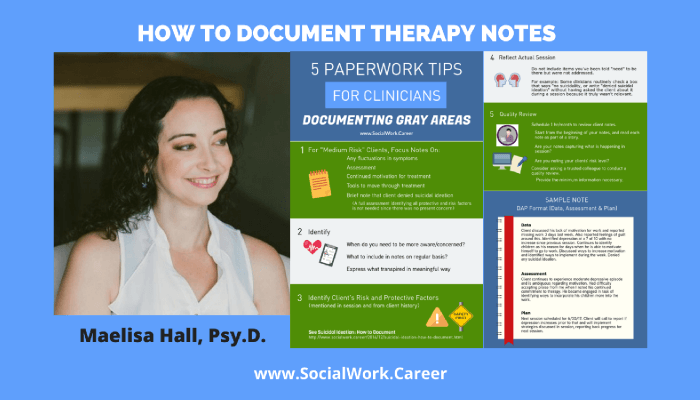
Not every therapy client is high-risk or worry-free—most fall somewhere in between. These “medium risk” situations include ongoing depression, self-harm behaviors without suicidal intent, impulsivity, and substance use. They require consistent assessment but don’t typically warrant hospitalization. The challenge? Knowing what to document and how often. This guide provides five practical tips from clinical documentation expert Maelisa Hall for managing therapy notes with medium risk clients. You’ll learn how to identify what’s truly relevant to document (without writing excessive notes), see a real DAP note example for a client with moderate depression, and discover why reviewing your documentation monthly can transform your practice. Whether you’re a new clinician or experienced therapist, these strategies help you create meaningful, legally sound therapy notes without burning out on paperwork
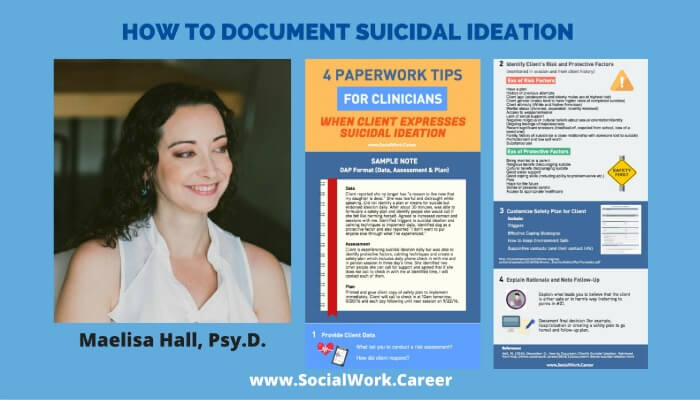
Suicidal Ideation: How to Document
When a client expresses suicidal ideation, documentation becomes crucial but also anxiety-inducing for many clinicians. Learn the four key components of effective suicide risk assessment documentation: providing clear client data with exact quotes, identifying risk and protective factors, creating safety plans (not contracts), and explaining your clinical rationale. This guide includes a sample progress note using the DAP format and best practices for follow-up documentation. Whether you’re a new clinician or experienced practitioner, these principles will help you create ethically sound documentation that protects both you and your clients while improving clinical practice.
Suicide Prevention: Take Five – You’re Worth It!
Take Five – You’re Worth It! To those of you who feel utterly hopeless, Overwhelmed, think there is no way out, Or see nothing to look forward to, I ask you to take a few minutes, To consider another possible solution, Than that of ending your life… There are people who love you, There are […]